This material is intended for people without medical education who want to know more about osteochondrosis than what is written in popular publications and on the websites of private clinics. Patients ask doctors of various specialties questions that characterize the complete misunderstanding of the topic of osteochondrosis. Examples of such questions are: "why does osteochondrosis hurt me? ", "congenital osteochondrosis was detected, what should I do? "Perhaps the apotheosis of such illiteracy can be considered a fairly common question: "Doctor, I have the initial signs of chondrosis, how terrible is this? "the article aims to structure the material about osteochondrosis, its causes, manifestations, methods of diagnosis, treatment and prevention, and to answer the most frequently asked questions. Since all of us, without exception, are patients with osteochondrosis, this article will be useful to everyone.
What is osteochondrosis?
The name of the disease is scary when it is not clear. The medical suffix "-oz" means the proliferation or increase of a tissue: hyalinosis, fibrosis. An example would be cirrhosis of the liver, when the connective tissue grows and the functional tissue, the hepatocytes, decreases in volume. There can be a buildup of a pathological protein, or amyloid, that should not otherwise be present. This storage disease will then be called amyloidosis. There may be significant enlargement of the liver due to fatty degeneration, called fatty hepatosis.
Well, it turns out that with intervertebral osteochondrosis, the cartilage tissue of the intervertebral discs increases in volume, because "chondros, χόνδρο" in translation from Greek to Russian means "cartilage"? No, chondrosis or, more precisely, osteochondrosis is not a storage disease. In this case, there is no real growth of the cartilage tissue, it is only a change in the configuration of the intervertebral cartilage discs under the influence of many years of physical activity, and we have previously examined what happens on each individual disc. The term "osteochondrosis" was introduced into the clinical literature by A. Hilderbrandt in 1933.
How does the biomechanics of a dehydrated disc change its shape? As a result of excessive loading, their outer edges swell, crack and bulge, then intervertebral hernias or cartilaginous nodules that protrude beyond the normal contour of the disc. That's why chondrosis is called chondrosis, because cartilage nodes - hernias - occur where cartilage should not be, behind the outer contour of a healthy disc.
The edges of the vertebrae, which are adjacent to the disc, also hypertrophy, forming coracoids or osteophytes. Therefore, such a mutual violation of the configuration of cartilage and bone tissue is collectively called osteochondrosis.
Osteochondrosis refers to dystrophic-degenerative processes and is part of the normal, normal aging of the intervertebral discs. None of us are surprised that the face of a 20-year-old girl will be slightly different from the face of a 70-year-old, but for some reason everyone believes that the spine, its intervertebral discs, are not subjected to the same pronounced temporary change. Dystrophy is a nutritional disorder, and degeneration is a disruption of the structure of the intervertebral discs that accompanies a long period of dystrophy.
Causes of osteochondrosis and its complications
The main cause of uncomplicated, physiological osteochondrosis can be considered the way a person moves: upright walking. Man is the only species on earth that walks on two legs among all mammals and this is the only way to move. Osteochondrosis has become a scourge of humanity, but we freed our hands and created civilization. Thanks to upright walking (and osteochondrosis), not only did we create the wheel, the alphabet, and conquer fire, but you can sit at home in the warmth of your home and read this article on your computer screen.
The closest relatives of humans, higher primates - chimpanzees and gorillas, sometimes get up on two legs, but this way of movement is auxiliary to them, and most often they still move on four legs. In order for osteochondrosis to disappear, like intensive aging of the intervertebral discs, a person needs to change the way of movement and remove the constant vertical load from the spinal column. Dolphins, killer whales and cetaceans do not have osteochondrosis, and dogs, cows and tigers do not. Their spine cannot withstand long-term static and shock vertical loads, because it is in a horizontal state. If humanity goes to sea, like Ichthyander, and the natural way of movement is diving, then osteochondrosis will be defeated.
The upright posture forced the human musculoskeletal system to evolve in the direction of protecting the skull and brain from impact loads. But the discs - the elastic cushions between the vertebrae - are not the only means of protection. A person has an elastic arch of the foot, cartilage of the knee joints, physiological curves of the spine: two lordosis and two kyphosis. All this allows you not to "shake" the brain even while running.
Risk factors
But doctors are interested in those risk factors that can be modified and avoid the complications of osteochondrosis, which cause pain, discomfort, limited mobility and reduced quality of life. Let's take a look at these risk factors, which are so often ignored by doctors, especially in private medical centers. After all, it is much more profitable to constantly treat a person than to point out the cause of the problem, solve it and lose the patient. here they are:
- the presence of longitudinal and transverse flat feet. Flat feet cause the arch of the foot to stop growing and the impact is transferred up the spine without softening. Intervertebral discs experience significant stress and quickly collapse;
- overweight and obesity - no comment needed;
- improper lifting and carrying of heavy objects, with uneven pressure on the intervertebral discs. For example, if you lift and carry a bag of potatoes on one shoulder, then the intense load will fall on one edge of the discs and may be excessive;
- physical inactivity and sedentary lifestyle. It was said above that it is during sitting that the maximum pressure on the discs occurs, because a person never sits straight, but always "slightly" bends;
- chronic injuries, ice skating, intense weight lifting, contact martial arts, heavy hats, hitting your head on low ceilings, heavy clothing, carrying heavy bags.
The risk factors that can affect each person are listed above. We deliberately do not list diseases here - connective tissue dysplasia, scoliotic deformation that changes the biomechanics of movement, Perthes disease and other conditions that complicate and worsen the course of physiological osteochondrosis and lead to complications. These patients are treated by an orthopedist. What are the common symptoms of complicated osteochondrosis that patients turn to doctors for?
General symptoms
The symptoms that will be described below exist outside of localization. These are common symptoms and can exist anywhere. These are pain, movement disorders and sensory disorders. There are also vegetative-trophic disorders, i. e. specific symptoms, for example, urination disorders, but much less often. Let's take a closer look at these signs.
Pain: muscular and radicular
Pain can be of two types: radicular and muscular. Radicular pain is associated with compression, i. e. pressing the protrusion or herniation of the intervertebral disc of the corresponding root at this level. Each nerve root consists of two parts: sensitive and motor.
Depending on where exactly the hernia is directed and which part of the root is compressed, sensory or motor disturbances may occur. Sometimes both disorders appear at once, expressed in different degrees. Pain also belongs to sensory disorders, because pain is a special, specific feeling.
Radicular pain: compressive radiculopathy
Radicular pain is known to many, it is called "neuralgia". The swollen nerve root reacts violently to every shock, and the pain is very sharp, similar to an electric shock. Shoots either the arm (from the neck) or the leg (from the lower back). Such a sharp, painful impulse is called lumbago: in the lower back it is lumbago, in the neck it is cervicago, a less common term. Such radicular pain requires forced, analgesic or antalgic posture. Radicular pain occurs immediately when coughing, sneezing, crying, laughing or straining. Any blow to the swollen nerve root causes increased pain.
Muscle pain: myofascial-tonic
But an intervertebral hernia or disc defect may not compress the nerve root, but may injure the nearby ligaments, fascia and deep muscles of the back during movement. In that case, the pain will be secondary, painful, permanent, there will be stiffness in the back, and such pain is called myofascial. The source of this pain will no longer be the nervous tissue, but the muscles. A muscle can respond to any stimulus in only one way: by contracting. And if the stimulus is prolonged, the muscle contraction will turn into a constant spasm, which will be very painful.
A vicious circle is formed: the cramping muscle cannot be well supplied with blood, becomes starved of oxygen and poorly removes lactic acid, i. e. the product of its own vital activity, into the venous capillaries. And the accumulation of lactic acid again leads to increased pain. This kind of chronic muscle pain significantly worsens the quality of life and forces the patient to undergo long-term treatment for osteochondrosis, although it does not prevent him from moving and does not force him to lie in bed.
A characteristic symptom of such secondary myofascial pain will be increased stiffness in the neck, lower back or thoracic spine, the appearance of dense, painful muscle lumps - "rollers" next to the spine, i. e. paravertebral. In such patients, the back pain intensifies after several hours of "office" of work, with prolonged immobility, when the muscles are practically unable to work and are in a state of spasms.
Diagnosis of osteochondrosis
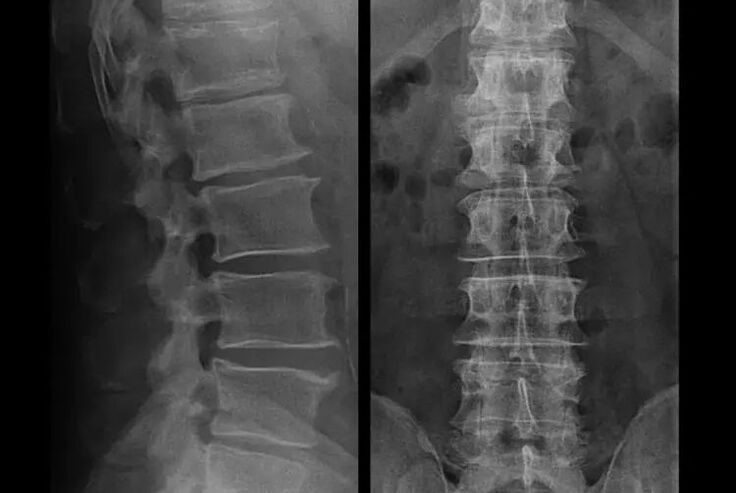
In typical cases, osteochondrosis of the cervical and cervical-thoracic spine occurs as described above. Therefore, the main stage of diagnosis was and remains the identification of the patient's complaints, determining the presence of accompanying muscle spasm by simple palpation of the muscles along the spinal column. Is it possible to confirm the diagnosis of osteochondrosis with an X-ray examination?
An "X-ray" of the cervical spine, even with functional tests for flexion and extension, does not show cartilage, because their tissue allows X-rays to pass through. Nevertheless, based on the location of the vertebrae, general conclusions can be drawn about the height of the intervertebral discs, the general correction of the physiological curvature of the neck - lordosis, as well as the presence of marginal growths on the vertebrae with prolonged irritation of their surfaces by fragile and dehydrated intervertebral discs. Functional tests can confirm the diagnosis of instability in the cervical spine.
Since discs can only be seen with CT or MRI, magnetic resonance and X-ray computed tomography are indicated to clarify the internal structure of the cartilage and formations such as protrusions and hernias. Thus, with the help of these methods, the diagnosis is accurately established, and the findings of the tomography are an indication, and even a topical guide, for the surgical treatment of the hernia in the department of neurosurgery.
It should be added that no other research method than imaging, except for MRI or CT, can show a hernia. So, if you have been given a modern "computer diagnosis" of the whole body, if a chiropractor has diagnosed a hernia by running your fingers along your back, if a hernia has been discovered on the basis of acupuncture, a special extrasensory technique or a session of Thai massage with honey, then you can immediately consider this level of diagnosis completelyilliterate. Complications of osteochondrosis caused by protrusion or hernia, compression, muscular, neurovascular, can only be treated by looking at the state of the intervertebral disc at the appropriate level.
Treatment of complications of osteochondrosis
Let us repeat once again that it is impossible to cure osteochondrosis, like planned aging and dehydration of the disc. You just can't let things get complicated:
- if there are symptoms of narrowing of the height of the intervertebral discs, then you need to move properly, do not gain weight and avoid the appearance of protrusions and pain in the muscles;
- if you already have a protrusion, then you must be careful not to rupture the fibrous ring, that is, not to transform the protrusion into a hernia and to avoid the appearance of protrusions at several levels;
- if you have a hernia, you must dynamically monitor it, regularly do magnetic resonance imaging, avoid increasing its size or carry out modern minimally invasive surgical treatment, because all conservative methods of treatment of exacerbation of osteochondrosis, without exception, leave the hernia in place and remove only temporary symptoms: inflammation, pain, cracking and muscle spasms.
But with the slightest violation of the regime, with heavy lifting, hypothermia, injury, weight gain (in the case of the lower back), the symptoms return again and again. We will describe how you can cope with unpleasant sensations, pains and limited mobility in the back against the background of worsening osteochondrosis, and the existing protrusion or hernia, secondary to social tonic syndrome.
What to do during an exacerbation?
Since an attack of acute pain has occurred (for example, in the lower back), it is necessary to adhere to the following instructions in the pre-medical phase:
- completely eliminate physical activity;
- sleeping on a hard (orthopedic mattress or hard sofa), eliminating back relaxation;
- it is advisable to wear a semi-rigid corset to prevent sudden movements and "distortions";
- A massage pillow with plastic needle applicators or a Lyapko applicator should be placed on the lower back. Keep it for 30 - 40 minutes, 2 - 3 times a day;
- after that, ointments containing NSAIDs, ointments with bee or snake venom can be rubbed into the lower back;
- after rubbing, on the second day you can wrap the lower back with dry heat, for example, with a dog hair belt.
A common mistake is warming up on the first day. This could be a heating pad, bathing procedures. At the same time, the swelling only increases, along with the pain. You can apply heat only after the "highest point of pain" has passed. After that, the heat will enhance the "resorption" of the swelling. This usually happens in 2-3 days.
The basis of any treatment is etiotropic therapy (removal of the cause) and pathogenetic treatment (influence on disease mechanisms). It is followed by symptomatic therapy. For vertebrogenic pain (caused by problems in the spine), things are like this:
- In order to reduce muscle and spine swelling, a salt-free diet and limiting the amount of fluid intake is indicated. You can even give a mild potassium-sparing diuretic tablet;
- in the acute phase of lumbar osteochondrosis, short-term treatment can be carried out with intramuscular "injections" of NSAIDs and muscle relaxants: daily, 1. 5 ml intramuscularly for 3 days, 1 ml also intramuscularly for 5 days. This will help relieve swelling of nerve tissue, remove inflammation and normalize muscle tone;
- in the subacute period, after overcoming the maximum pain, you should no longer take "injections", and you should pay attention to restorative agents, for example, modern drugs of group "B". They effectively restore impaired sensitivity, reduce numbness and paresthesias.
Physiotherapy measures continue, it's time for exercise therapy for osteochondrosis. Its task is to normalize circulation and muscle tone, when the swelling and inflammation have already subsided, but the muscle spasm has not yet been completely resolved.
Kinesiotherapy (movement treatment) includes performing therapeutic exercises and swimming. Gymnastics for osteochondrosis of the cervical spine is not aimed at the discs at all, but at the surrounding muscles. Its task is to relieve tonic spasm, improve blood flow, and also normalize venous outflow. This is what leads to a decrease in muscle tone, a decrease in pain and stiffness in the back.
Along with massage, swimming and acupuncture, it is recommended to buy an orthopedic mattress and a special pillow. A pillow for osteochondrosis of the cervical spine should be made of a special "shape memory" material. Its task is to relax the muscles of the neck and suboccipital region, as well as to prevent blood flow disturbances at night in the vertebrobasilar region.
Autumn is an important phase in the prevention and treatment of home physiotherapy products and devices - from infrared and magnetic devices, to the most common needle applicators and ebonite discs, which are the source of weak electric currents during massage that have a beneficial effect on the patient.
Exercises for osteochondrosis must be performed after a light general warm-up, on "warmed-up muscles". The main therapeutic factor is movement, not the degree of muscle contraction. Therefore, in order to avoid relapse, the use of weights is not allowed; With their help, you can effectively restore range of motion.
The rubbing of ointment and the use of the Kuznetsov implicator continue. Bathing, underwater massage, Charcot shower are shown. In the worsening phase, drugs for home magnetotherapy and physiotherapy are indicated.
Usually, the treatment does not last longer than a week, but in some cases, osteochondrosis can manifest itself with such dangerous symptoms that an operation may be needed, and that urgently.
About Shant's collar
In the early stages, during the acute phase, it is necessary to protect the neck from unnecessary movements. Shants collar is great for this. Many people make two mistakes when buying this collar. They do not choose it according to size, because of which it simply does not perform its function and causes a feeling of discomfort.

Another common mistake is long-term wearing for prophylactic purposes. This weakens the neck muscles and only causes more problems. For the necklace, there are only two indications under which it can be worn:
- the appearance of acute pain in the neck, stiffness and pain that spreads to the head;
- if you are going to do physical work while you are in full health, where there is a risk of "straining" the neck and getting worse. This is, for example, repairing a car, when you lie down under it, or washing windows, when you need to reach out and take awkward positions.
The collar should be worn for no longer than 2-3 days, because longer wear can cause venous congestion in the neck muscles, at a time when it is time to activate the patient. An analogue of the Shants collar for the lower back is a semi-rigid corset purchased in an orthopedic salon.
Surgical treatment or conservative measures?
It is recommended that every patient, after the progression of symptoms, in the presence of complications, undergo MRI and consult a neurosurgeon. Modern minimally invasive operations allow the safe removal of rather large hernias, without prolonged hospitalization, without forcing or lying down for several days, without impairing the quality of life, because they are performed with modern video endoscopic, radiofrequency, laser technology or using cold plasma. You can vaporize part of the core and reduce the pressure, reducing the risk of developing a hernia. And you can radically eliminate the defect, that is, get rid of it completely.
There is no need to be afraid to operate on hernias, it is no longer the previous type of open surgery in the 80s-90s of the last century with muscle dissection, blood loss and subsequent long recovery period. They are more like a small puncture under X-ray control followed by the use of modern technology.
If you prefer a conservative method of treatment, without surgery, then know that no method will allow you to reduce or eliminate the hernia, no matter what they promise you! Neither hormone injection, nor electrophoresis with papain, nor electrical stimulation, nor massage, nor the use of leeches, nor acupuncture can deal with a hernia. Neither creams and balms, kinesiotherapy, nor even the introduction of platelet-rich plasma will help. And even traction therapy, or traction, for all its benefits, can only reduce symptoms.
Therefore, the motto for the conservative treatment of intervertebral hernias can be the well-known expression "minced meat cannot be returned". The hernia can be eliminated only quickly. The prices for modern business are not so high, because they have to be paid once. ultimately cost 10-20 times more than the radical removal of the hernia with the disappearance of pain and restoration of the quality of life.
Prevention of osteochondrosis and its complications
Osteochondrosis, including the complicated ones, about the symptoms and treatment of which we discussed above, is mostly not a disease, but simply a manifestation of inevitable aging and premature "reduction" of the intervertebral discs. Osteochondrosis needs a little to never disturb us:
- avoid hypothermia, especially in autumn and spring, and autumn winter;
- do not lift weights and carry loads only with a straight back, in a backpack;
- drink more clean water;
- do not gain weight, your weight should correspond to your height;
- treat flat feet, if any;
- do physical exercises regularly;
- engaging in types of exercises that reduce the load on the back (swimming);
- giving up bad habits;
- alternating mental stress with physical activity. After every hour and a half of mental work, it is recommended to change the type of activity to physical work;
- You can regularly do at least an X-ray of the lumbar spine in two projections, or an MRI, to know if the hernia, if any, is progressing;
By following these simple recommendations, you can keep your back healthy and mobile for life.























